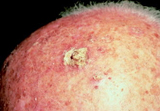
 Actinic keratoses (AKs) are dry, scaly patches that form on sun exposed areas of the skin, including the scalp, face, forearms, and back of the hands. A single lesion is called an "actinic keratosis" or "solar keratosis".
Actinic keratoses (AKs) are dry, scaly patches that form on sun exposed areas of the skin, including the scalp, face, forearms, and back of the hands. A single lesion is called an "actinic keratosis" or "solar keratosis".
Actinic keratoses are usually scaly, feel like sandpaper to the touch, and range in color from skin-toned to reddish-brown. Actinic keratoses may be as small as the head of a pin or as large as a quarter (or bigger, if left untreated).
Most people with one actinic keratosis (AK) lesion will develop others. Actinic keratoses can appear in groups and many may be undetected. They may occasionally itch or become tender, especially after sun exposure.
When actinic keratoses occur on the lip, they are referred to as actinic cheilitis. This type of AK appears as cracking, dried lips, often around the border of the lip.
Actinic Keratoses and Skin Cancer
Actinic keratoses are considered PRECANCEROUS by many physicians and have the potential to become a type of skin cancer called squamous cell carcinoma (SCC). In fact, 40-60% of squamous cell skin cancers begin as untreated AKs.
Therefore, your doctor will be diligent in diagnosing, treating, and monitoring actinic keratoses. Also, since actinic keratoses result from chronic sun exposure, those with AKs are at risk for developing other types of skin cancer, such as basal cell carcinoma or melanoma.
Fortunately, actinic keratoses are treatable when detected in the early stages. People at risk for actinic keratoses and skin cancer can reduce that risk by performing frequent skin self-exams and seeing their doctor for regular screenings.
Risk Factors for Developing Actinic Keratoses (AKs)
Actinic keratoses usually develop in people with light-colored skin and hair (blond or red hair), have freckles and have years of excessive sun exposure.
Actinic keratoses are most common in men and women over 40 years old. However, even younger people (including those with dark skin) can develop actinic keratoses if they live in very sunny climates.
People with weakened immune systems due to underlying illness or the use of immunosuppressive medications, such as chemotherapy, are much more likely to develop AKs.
Treatment Options for Actinic Keratoses
There are many actinic keratosis treatment options. After diagnosing your actinic keratoses, your doctor will consider these factors:
- The number, size, and location of actinic keratoses lesion(s)
- Results of past treatments, if treated before
- Your age and medical history, such immune system function
- Your personal preferences
Before choosing a treatment, your doctor may recommend a skin biopsy to be sure that your lesions aren't cancerous. This is done by removing all or part of the actinic keratoses and examining the tissue under a microscope.
 Topical Medications for Actinic Keratoses
Topical Medications for Actinic Keratoses
There are several safe and effective medications for the treatment of actinic keratoses. All of these are applied to the skin and available by prescription-only.
Medications approved for the treatment of actinic keratoses include the following:
- 5-fluorouracil or "5-FU" (Carac® or Efudex®)
- Imiquimod, 5% (generic. Formerly referred to as Aldara®)
- Picato® Gel (ingenol mebutate)
- Solaraze® (diclofenac sodium - 3%)
- Zyclara™ (imiquimod) Cream, 3.75%
Each of these medications must be applied regularly as prescribed, over several days or weeks.
Your personal treatment regimen may vary depending on the medication prescribed, the area to which it is applied, the number of lesions being treated, and your ability to tolerate any irritation or other side effects. This makes it very important to closely follow your doctors’s specific instructions.
Procedures to Treat Actinic Keratoses
Several dermatologic procedures are effective for actinic keratosis treatment. Your doctor will recommend a procedure that is best suited to the location of the actinic keratoses and other variables. These procedures may be combined with other actinic keratosis treatments or medications.
- Cryosurgery uses liquid nitrogen to freeze off the lesions. It is fast, has a high cure rate, and is well-tolerated by most people. There may be a very brief period of stinging when the liquid nitrogen is first applied, but anesthesia is not required.
- Shave removal is a procedure during which a scalpel is used to remove the lesion and obtain a specimen for testing.
- Curettage is often used to remove hard, thickened actinic keratoses. In this procedure, a small, round, sharp instrument (called a curette) is used to scrape the actinic keratosis, either removing a piece of it for biopsy or removing the entire lesion.
- Lasers deliver an intense light focused on the lesion, removing it along with the top layer of skin. The finely controlled nature of laser removal makes this a useful option for actinic keratoses on delicate skin, such as the lips (actinic chelitis), or in narrow, hard-to-reach places (such as behind the ears).
- Photodynamic therapy uses a substance that is applied to the skin that makes the AK lesions very sensitive to light. A laser or light is then directed onto the skin that destroys the lesions.
Key Points About Actinic Keratosis Treatment
- Be patient. Some actinic keratosis treatments take longer than others, and some actinic keratoses may require more than one treatment.
- During treatment, actinic keratoses may look worse before they look better. Some medications will make actinic keratoses appear that weren’t previously visible.
- Be aware that your insurance company may require a higher co-payment for some medications or procedures. These higher costs may be offset by shorter healing time or other desired outcomes.
Whether your treatment is an in-office procedure that takes just an hour or a topical regimen that lasts several weeks, your doctor will monitor your skin’s condition to make sure the treatment is working and that side effects are manageable.
Talk to your doctor if you are concerned about any side effects that you experience.
Actinic Keratoses Skin Care Tips
- AVOID SUN EXPOSURE. The best way to avoid new actinic keratoses and skin cancer is to protect your skin from the sun and the damaging ultraviolet (UV) rays. If you can’t avoid spending time outdoors, make sun protection a priority. Use a broad-spectrum sunscreen with a minimum SPF of 30, and cover your skin with long-sleeved shirts, pants, and a wide-brimmed hat.
- Avoid indoor tanning. Indoor tanning beds also expose the skin to damaging UV rays that increase the risk of developing AKs and skin cancer.
- Perform skin self-exams. As someone who has already been diagnosed with an actinic keratosis, you are likely to develop more actinic keratoses over time—therefore, it’s important to schedule yearly skin exams with your doctor. You may also be advised to perform regular skin self-exams. The goal is not only to detect new actinic keratoses but also to check for changes in existing skin lesions, such as bleeding or a change in size.
Source: Vivacare
Last updated : 12/13/2021