What’s an IUD?
An IUD is a tiny device that's put into your uterus to prevent pregnancy. It’s long-term, reversible, and one of the most effective birth control methods out there.
What does IUD stand for?
IUD stands for Intrauterine Device (basically: a device inside your uterus). It's a small piece of flexible plastic shaped like a T. Sometimes it’s called an IUC — intrauterine contraception.
What are the types of IUDs?
There are 5 different brands of IUDs that are FDA approved for use in the United States:
- Paragard,
- Mirena,
- Kyleena,
- Liletta, and
- Skyla.
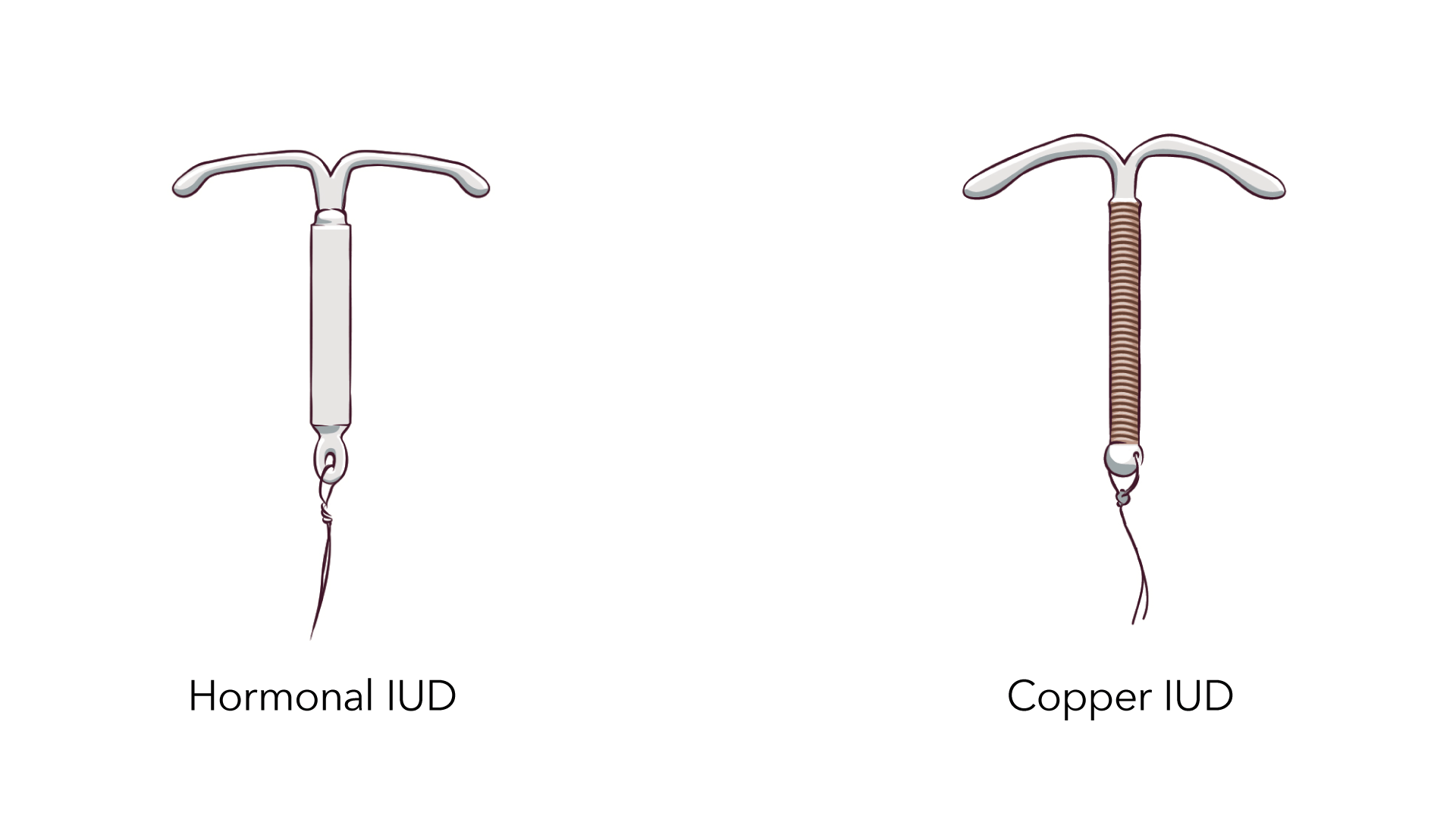
These IUDs are divided into 2 types:
- hormonal IUDs (Mirena, Kyleena, Liletta, and Skyla).
- copper IUDs (Paragard) and
The Paragard IUD doesn’t have hormones. It’s wrapped in a tiny bit of copper, and it protects you from pregnancy for up to 12 years.
The Mirena, Kyleena, Liletta, and Skyla IUDs use the hormone progestin to prevent pregnancy. Progestin is very similar to the hormone progesterone that our bodies make naturally. Mirena works for up to 8 years. Kyleena works for up to 5 years. Liletta works for up to 8 years. Skyla works for up to 3 years.
How do IUDs work?
Both copper IUDs and hormonal IUDs prevent pregnancy by changing the way sperm cells move so they can't get to an egg. If sperm can’t make it to an egg, pregnancy can’t happen.
The Paragard IUD uses copper to prevent pregnancy. Sperm doesn’t like copper, so the Paragard IUD makes it almost impossible for sperm to get to that egg.
The hormones in the Mirena, Kyleena, Liletta, and Skyla IUDs prevent pregnancy in two ways: 1) they thicken the mucus that lives on the cervix, which blocks and traps the sperm, and 2) the hormones also sometimes stop eggs from leaving your ovaries (called ovulation), which means there’s no egg for a sperm to fertilize. No egg, no pregnancy.
One of the awesome things about IUDs is that they last for years — but they’re not permanent. If you decide to get pregnant or you just don’t want to have your IUD anymore, your nurse or doctor can quickly and easily take it out. You’re able to get pregnant right after the IUD is removed.
Can IUDs be used as emergency contraception?
Yes! The Paragard, Mirena, and Liletta IUDs work super well as emergency contraception. If you get one of these IUDs put in within 120 hours (5 days) after unprotected sex, it’s more than 99% effective. It’s actually the most effective way to prevent pregnancy after sex.
Another great thing about using an IUD as emergency contraception: you can keep it and have really effective birth control that you can use for up to 8 to12 years (depending on which kind you get). The other kind of emergency contraception is the morning-after pill. You can take it up to 5 days after unprotected sex to reduce the risk of pregnancy.
How effective are IUDs?
The IUD is almost mistake-proof, making it one of the most effective methods available.
How effective are IUDs when used as birth control?
IUDs are one of the best birth control methods out there — more than 99% effective. That means fewer than 1 out of 100 people who use an IUD will get pregnant each year.
IUDs are so effective because there's no chance of making a mistake. You can’t forget to take it (like the pill), or use it incorrectly (like condoms). And you're protected from pregnancy 24/7 for 3 to 12 years, depending on which kind you get. Once your IUD is in place, you can pretty much forget about it until it expires. You can keep track of your insertion and removal date using our birth control app.
How effective are IUDs when used as emergency contraception?
The Paragard (copper), Mirena, and Liletta IUDs are the most effective method of emergency contraception available. If you get one of these IUDs put in within 120 hours (5 days) after having unprotected sex, it’s more than 99.9% effective at preventing pregnancy. Then, if you want to, you can keep it and have really effective birth control that you can use for up to 8 to 12 years (depending on which kind you get).
Do IUDs protect against STDs?
No, IUDs don't protect against STDs. Luckily, using condoms or internal condoms every time you have sex does lower the chance of getting or spreading STDs. So using condoms with your IUD is the way to go.
How can I get an IUD?
You can get an IUD from your local Planned Parenthood health center or another nurse or doctor. You may be able to get an IUD for free or at low cost.
How much does an IUD cost?
Getting an IUD costs anywhere between $0 to $1,300. That’s a pretty wide range, but the good news is that IUDs can be free or low cost with many health insurance plans, Medicaid, and some other government programs.
Prices can also vary depending on which kind you get. The price of an IUD includes medical exams, getting the IUD put in, and follow-up visits.
Even if an IUD costs more than other methods up front, they usually end up saving you money in the long run because they last for years.
If you’re worried about cost, check with your local Planned Parenthood health center to see if they can hook you up with birth control that fits your budget.
Can I get an IUD for free or low-cost?
There's a good chance you can get an IUD for free (or for a reduced price) if you have health insurance. Because of the Affordable Care Act (aka Obamacare), most insurance plans must cover all methods of birth control, including IUDs.
However, some plans don’t cover all brands of IUDs. Your health insurance provider can tell you which ones they pay for. Your doctor may also be able to help you get your birth control method of choice covered by health insurance.
If you don't have health insurance, you've still got options. Depending on your income and legal status in the U.S., you may qualify for Medicaid or other state programs that can help you pay for birth control and other health care.
Planned Parenthood works to provide you with the services you need, whether or not you have insurance. Most Planned Parenthood health centers accept Medicaid and health insurance, and many charge less for services and birth control depending on your income.
Where do I go to get an IUD?
An IUD has to be put in by a doctor, nurse, or other health care provider. You can contact your gynecologist, family planning clinics, or a local Planned Parenthood health center to find out more about getting an IUD.
What's an IUD insertion like?
A doctor or nurse puts the IUD in through your vagina and into your uterus. Some people feel cramps or pain, but it doesn't last long and medicine can help.
How is an IUD put in?
First, your nurse or doctor will ask you some questions about your medical history. Then they’ll check your vagina, cervix, and uterus, and they may test you for STDs. You may be offered medicine to help open and/or numb your cervix before the IUD is put in.
To put the IUD in, the nurse or doctor will put a speculum into your vagina and then use a special inserter to put the IUD in through the opening of your cervix and into your uterus. The process usually takes less than five minutes.
IUDs can be put in at any point in your menstrual cycle, and you can usually get one put in right after giving birth or having an abortion.
How does it feel to get an IUD put in?
People usually feel some cramping or pain when they're getting their IUD placed. The pain can be worse for some, but luckily it only lasts for a minute or two.
Some doctors tell you to take pain medicine before you get the IUD to help prevent cramps. They also might inject a local numbing medicine around your cervix to make it more comfortable.
Some people feel dizzy during or right after the IUD is put in, and there's a small chance of fainting. You might want to ask someone to come with you to the appointment so you don't have to drive or go home alone, and to give yourself some time to relax afterward.
What can I expect after an IUD insertion procedure?
Many people feel perfectly fine right after they get an IUD, while others need to take it easy for a while. There can be some cramping and backaches, so plan on chilling at home after your appointment — it’s a great excuse to curl up on the couch with your favorite book or movie. Heating pads and over-the-counter pain meds can help ease cramps too.
You may have cramping and spotting after getting an IUD, but this almost always goes away within 3-6 months. Hormonal IUDs eventually make periods lighter and less crampy, and you might stop getting a period at all. On the flip side, copper IUDs may make periods heavier and cramps worse. For some people, this goes away over time. If your IUD is causing you pain, discomfort, or side effects you don’t like, call your doctor.
Once you get the IUD, a string about 1 or 2 inches long will come out of your cervix and into the top of your vagina; don’t worry, you won’t notice it. The string is there so a nurse or doctor can remove the IUD later. You can feel the string by putting your fingers in your vagina and reaching up toward your cervix. But DON’T tug on the string, because you could move your IUD out of place or pull it out.
There's a very small chance that your IUD could slip out of place. It can happen any time, but it's more common during the first 3 months. IUDs are most likely to come out during your period. Check your pads, tampons, or cups to see if it fell out. You can also check your string to make sure it’s still there. If your IUD falls out, you’re NOT protected from pregnancy, so make sure to go see your doctor, and use condoms or another kind of birth control in the meantime.
Remember when you got your IUD (or write it down somewhere), so you’ll know when it needs to be replaced. The Paragard IUD should be replaced after 12 years. Mirena should be replaced after 8 years. Kyleena should be replaced after 5 years. Liletta should be replaced after 8 years. Skyla should be replaced after 3 years.
How soon after getting an IUD can I have sex?
You can have sex as soon as you want after getting an IUD.
You might need to use a backup method of birth control (like condoms) until the IUD starts to work — whether you're protected against pregnancy right away depends on what type of IUD you get and when it’s put in your uterus.
Paragard (copper), Mirena, and Liletta IUDs start working to prevent pregnancy as soon as they're in place.
Kyleena and Skyla IUDs start working to prevent pregnancy right away IF they’re put in during the first 7 days of your period. If you get a Kyleena or Skyla IUD at any other time during your cycle, protection starts after 7 days — in the meantime, use condoms or another kind of birth control to prevent pregnancy.
What are the side effects of IUDs?
Hormonal IUD side effects and copper IUD side effects are different. Cramps and spotting with the IUD are common at first. But many IUD side effects go away or get less noticeable within a few months. And some IUD side effects are positive.
What hormonal IUD side effects should I expect?
Hormonal IUDs (like Mirena, Kyleena, Liletta, and Skyla) can cause side effects. But for most people, that’s actually a good thing — the most common hormonal IUD side effects usually help make your periods better.
Hormonal IUDs can cut down on cramps and PMS, and they usually make your periods much lighter. Some people stop getting their periods at all while they have their IUD (don’t worry, this is totally normal and safe). In fact, many people get hormonal IUDs to help with heavy or painful periods, to treat symptoms of endometriosis or PCOS, or because they just don’t want to bleed every month.
Other hormonal IUD side effects can include:
-
Pain when the IUD is put in, and cramping or back aches for a few days after
-
spotting between periods
-
irregular periods
These usually go away within 3–6 months, once your body gets used to the new visitor in your uterus. And they don’t happen to everyone — many people use hormonal IUDs with no problems at all.
Over-the-counter pain medicine (like ibuprofen, naproxen, or aspirin) can usually help with IUD cramps. If you have cramping that doesn’t get better or is really painful, talk with your nurse or doctor. They may need to check to make sure that your IUD is in the right place.
The changes in your periods while you have your IUD can make some people worry about how they’ll know they’re not pregnant. But you don’t really need to worry about being pregnant even if you don’t get a period, because the IUD is really good at what it does — it’s more than 99% effective at preventing pregnancy.
If you do think you might be pregnant, take a pregnancy test and call your nurse or doctor right away if it’s positive. It’s very rare to get pregnant while you have an IUD, but if it does happen, it’s more likely to be an ectopic pregnancy, which can be dangerous and needs medical attention right away.
The hormones in these IUDs and other types of hormonal birth control (like the implant and shot) have been around for decades, and millions of people have used them safely. Hormonal IUD side effects aren’t dangerous, though there are some possible risks with using IUDs, like with any medicine. You can always call a nurse or doctor, like the ones at your local Planned Parenthood health center, if you have any concerns. And you can keep track of any side effects you may be having with our birth control app.
What copper IUD side effects should I expect?
The copper IUD (aka Paragard IUD) has no hormones, so you don’t have to deal with any of the risks or side effects that can sometimes happen with hormonal birth control methods.
But copper IUDs often cause more bleeding and cramps during your period, especially in the first 3-6 months. For many people, this gets better over time.
Paragard side effects can include:
-
spotting between periods
-
irregular periods
-
heavier or longer periods
-
more or worse cramping during your periods
-
pain when your IUD is put in, and cramping or back aches for a few days after
Over-the-counter pain medicine can help with IUD cramps. And the cramping and bleeding usually get better after a few months, once your body gets used to your IUD. You can keep track of any side effects you may be having with our birth control app.
Birth control shouldn’t make you feel uncomfortable. If you have bleeding or pain that really bothers you, talk with your nurse or doctor. They may need to check and make sure your IUD is in the right place, or they might recommend a different method of birth control for you. Some people try a few different birth control methods before finding the right one for them.
The copper IUD has been around for decades, and millions of people have used it safely, though there are some possible risks, like with any medical device. You can always call a nurse or doctor, like the ones at your local Planned Parenthood health center, if you have any concerns.
Are there IUD removal side effects?
You may have some spotting for a little while after your nurse or doctor takes out your IUD, but otherwise you should feel totally normal.
When you stop using an IUD, your body will eventually return to the way it was before you got it. So if your period got heavier on the copper IUD, it will go back to what was normal for you before you got the IUD. If you stopped getting your period on the hormonal IUD, your period will eventually come back after the IUD is out. It can take a few months for your period to go back to what’s normal for you.
An important thing to note: you can get pregnant right away once your IUD is out, even if your periods aren’t regular or haven’t come back yet. So if you have your IUD removed but you don’t want to get pregnant, make sure to use another birth control method.
Everyone’s body is different, and our bodies also change over time. So there’s no way to know exactly how your body will react to going off the IUD. But any side effects that you may have will go away within a few months as your body gets used to not having an IUD anymore.
If you’re really worried about the side effects of going off the IUD, talk with your nurse or doctor. They may be able to give you more specific information about what to expect based on your personal medical history.
How safe is the IUD?
The IUD is very safe for most people. Here's how to figure out if the IUD is safe for you.
Can I get an IUD?
Most people can use IUDs safely, but there are some conditions that make side effects or complications more likely. Talk to your nurse or doctor to find out if IUDs are safe for you.
You may not be able to get an IUD if you
-
have certain STDs or pelvic infection
-
think you might be pregnant
-
have cervical cancer that hasn't been treated
-
have cancer of the uterus
-
have had a pelvic infection after either childbirth or an abortion in the past 3 months
You also shouldn't get a Paragard IUD if you have a copper allergy, Wilson's Disease, or a bleeding disorder that makes it hard for your blood to clot. And you shouldn't get a hormonal IUD if you have had breast cancer.
Very rarely, the size or shape of someone’s uterus makes it hard to place an IUD correctly.
If you have a condition that rules out an IUD for you, don’t worry. You’ve got lots of other birth control options.
What are the risks of an IUD?
There are possible risks with an IUD, but serious problems are really rare.
The IUD can sometimes slip out of your uterus — it can come all the way out or just a little bit. If this happens, you can get pregnant. If the IUD only comes out part of the way, a nurse or doctor has to remove it.
Don’t use a menstrual cup with an IUD. Using a menstrual cup can cause your IUD to move out of place. If you do decide to use a menstrual cup, you need to check your IUD strings monthly, and contact your nurse or doctor if your IUD strings are missing.
It’s possible — though extremely unlikely — to get pregnant even if your IUD is in the right spot. If you get pregnant, a nurse or doctor will need to remove your IUD as soon as possible. If you get pregnant with an IUD in place, there’s an increased risk of ectopic pregnancy and other serious health problems.
It’s possible to get an infection if bacteria gets into your uterus when the IUD is put in. If the infection isn't treated, it may make it harder for you to get pregnant in the future.
When the IUD is put in, it could push through the wall of your uterus. This sounds painful, but it usually doesn't hurt. But if this happens, you may need surgery to remove the IUD. However, this is very rare.
What warning signs should I know about?
Chances are that you’ll have no problems with your IUD. But it's still important to pay attention to your body and how you feel after you get your IUD. Here are the warning signs to watch out for. Call your nurse or doctor right away if:
-
the length of your IUD string feels shorter or longer than it was
-
you can feel the hard plastic bottom of the IUD coming out through your cervix
-
you think you might be pregnant
-
you have bad cramping, pain, or soreness in your lower belly or stomach
-
there’s pain or bleeding during sex
-
you get unexplained fever, chills, or have trouble breathing
-
your vaginal discharge is different than normal
-
you have vaginal bleeding that is heavier than usual
If you have unprotected sex with someone who has an STD, see your nurse or doctor for any tests or treatments you may need.
Is it safe to use the IUD while breastfeeding?
Yes, it’s safe to use the IUD while you’re breastfeeding. It shouldn’t have any effect on how much milk you produce, and it won’t hurt your baby. In fact, the IUD is a great method to use if you’re breastfeeding and you don’t want to get pregnant.
What are the benefits of IUDs?
IUDs are one of the best ways to prevent pregnancy, and they last for years. You can get it, forget it, and still be protected.
IUDs are VERY effective.
IUDs give you great, long-term protection against pregnancy — they’re more than 99% effective. They work as well as sterilization and the birth control implant. IUDs are one of the most effective methods you can get because there’s almost no way you can mess it up. You can’t forget to use it (like the pill or ring), or use it incorrectly (like condoms). IUDs are “set-it-and-forget-it” birth control.
IUDs are REALLY convenient.
Once your IUD is in, you barely have to think about it — it works until it expires or you have it taken out. That means no trips to the pharmacy, no pill to take or ring to put in, and nothing you have to do before sex to prevent pregnancy. Plus you’re protected against pregnancy for 3 to 12 years, depending on what kind you get.
You can get pregnant after taking out an IUD.
IUDs are reversible. If you decide you want to get pregnant, you can get it removed at any time. IUDs won’t affect your fertility or make it harder to get pregnant in the future. In fact, it’s possible to get pregnant as soon as your IUD is out.
Hormonal IUDs can make your periods better.
Hormonal IUDs (Mirena, Kyleena, Liletta, and Skyla) can cut down on cramps and make your period way lighter. Some people totally stop getting periods at all. Hormonal IUDs can help treat people who suffer from severe cramps, really heavy periods, and anemia.
The copper IUD doesn’t have hormones.
Some people prefer non-hormonal birth control, or can’t use methods with hormones because of medical problems. Luckily, the Paragard (copper) IUD is super effective at preventing pregnancy AND totally hormone free.
IUDs can be used as emergency contraception.
The Paragard, Mirena, and Liletta IUDs are the most effective form of emergency contraception out there. If you get one of these IUDs put in within 120 hours (5 days) after unprotected sex, it’s more than 99% effective against pregnancy. And — bonus! — your IUD can keep preventing pregnancy for as long as you like, up to 8 -12 years (depending on which kind you get).
What are the disadvantages of IUDs?
Some people have side effects that bother them after getting an IUD, but these usually go away after a few months. Rarely, the side effects can be serious.
There can be some negative side effects.
Some people have side effects after getting an IUD. Hormonal IUDs and copper (non-hormonal) IUDs have different side effects.
Your side effects will probably ease up after about 3–6 months, once your body gets used to your IUD. So if you can stick it out for a few months, there’s a good chance any side effects you’re having will eventually go away or be less noticeable. You can keep track of any side effects you're experiencing with our birth control app. If you’re still having pain or other side effects that bother you after a while, or your side effects are really bad, talk with your nurse or doctor.
IUDs don’t protect against STDs.
While IUDs are one of the best ways to prevent pregnancy, they don't protect you from sexually transmitted infections. Luckily, using condoms every time you have sex reduces the chance of getting or spreading STDs. So the thing to do is to use condoms with your IUD.
There are some risks with the IUD, but they’re rare.
Serious problems from IUDs are not at all common, but there are some risks and warning signs to look out for.
IUD insertion can hurt, but the pain doesn’t last long
The process of getting your IUD placed can be painful for some people. It usually feels like strong period cramps. But the good news is, it’s really quick — the worst part is usually over in less than a minute, and then you’ve got really effective birth control that you don’t have to think about for several years. If you’re worried about pain, ask your nurse or doctor about medicine or other ways to help when you make your appointment.
Even if the insertion is not exactly a fun time, lots of IUD users think it’s totally worth it in the end. Hormonal IUDs usually make your periods much lighter and less crampy. And for people who can’t use or don’t want to use hormonal methods (but still want super-effective, non-permanent birth control), copper IUDs are a really great option. So many people are willing to deal with a few minutes of pain in exchange for years of really effective birth control along with the other benefits of IUDs.
How does IUD removal work?
Your IUD will protect you from pregnancy for 3 to 12 years, but your doctor or nurse can take it out any time before that if you like. Removal is simple.
How will it feel to get my IUD removed?
Getting your IUD taken out is pretty quick and simple. A health care provider gently pulls on the string, and the IUD’s arms fold up and it slips out. You may feel cramping for a minute as it comes out.
There’s a small chance that your IUD won’t come out easily. If this happens, your nurse or doctor may use special instruments to remove it. Very rarely, surgery may be needed.
When should I get my IUD removed?
You can get your IUD taken out whenever you want. If your IUD is going to expire but you still don’t want to get pregnant, you’ll have to replace it.
- Paragard should be replaced after 12 years.
- Mirena should be replaced after 8 years.
- Liletta should be replaced after 8 years.
- Kyleena should be replaced after 5 years.
- Skyla should be replaced after 3 years.
What should I expect after I get my IUD removed?
You should feel completely normal after getting your IUD taken out. You may have some light bleeding after IUD removal, and some slight cramping during and right after removal.
Any side effects that you may have had while you were on the IUD will eventually go away after your IUD is out. Unless you start a hormonal birth control method after getting your IUD out, your period will go back to how it was before you got your IUD. Read more about what side effects to expect after getting your IUD out.
How soon can I get pregnant after getting my IUD removed?
Your fertility goes back to normal right after your IUD is out, so it's possible to get pregnant right away. If you get your IUD removed and you don’t want to get pregnant, use another method of birth control.
Where can I get my IUD removed?
You can usually get your IUD removed at the same health center that put it in for you. But any nurse or doctor who puts in IUDs can also remove them. The nurses and doctors at Planned Parenthood health centers, family planning clinics, and private gynecologist offices can all do IUD removal. Use our health center locator to find a Planned Parenthood health center that offers IUD removal near you.
How much does it cost to get my IUD removed?
The price of IUD removal varies depending on where you go, costing anywhere from $0-$250. You might be able to get your IUD removed for free (or for a reduced price) if you have health insurance or qualify for certain programs.
Because of the Affordable Care Act (aka Obamacare), most health insurance plans must cover all doctor’s visits related to birth control, including IUD removal. You can call the number on the back of your health insurance card or talk with your nurse or doctor if you have questions. Learn more about health insurance and affordable birth control.
If you don't have health insurance, you still have options. Depending on your income and legal status in the U.S., you may be able to enroll in Medicaid or other programs that can help you pay for your IUD removal and other health care.
Planned Parenthood health centers work to provide you with the services you need, whether or not you have insurance. Most Planned Parenthood health centers accept Medicaid and health insurance, and many charge less for services depending on your income. If you need to get your IUD removed and you’re worried about cost, contact your local Planned Parenthood health center for more information about affordable IUD removal near you.
What are hormonal IUDs?
IUD stands for Intrauterine Device — a birth control method that sits inside your uterus. A hormonal IUD is a small piece of flexible plastic shaped like a T. The hormonal IUD releases a tiny amount of the hormone progestin into your body over several years. Progestin is very similar to the hormone progesterone that our bodies make naturally.
The hormones in the IUD help prevent pregnancy, and can also help with painful or heavy periods while you’re using it.
Hormonal IUDs prevent pregnancy by keeping sperm cells away from your eggs. If sperm can’t make it to an egg, pregnancy can’t happen. The hormones in the IUD prevent pregnancy in two ways:
1) Hormonal IUDs make the mucus on your cervix thicker. This mucus blocks sperm so it can’t get to an egg.
2) The hormones in the IUD can also stop eggs from leaving your ovaries (called ovulation), which means there’s no egg for a sperm to fertilize. No egg = no pregnancy.
One of the awesome things about IUDs is that they last for years, but they’re not permanent. If you decide that you want to get pregnant, or if you just don’t want to have your IUD anymore, your nurse or doctor can take it out. After you get your IUD removed, your fertility goes back to what's normal for you.
What are the kinds of hormonal IUDs?
There are four brands of hormonal IUDs available in the U.S.: Mirena, Kyleena, Liletta, and Skyla. They all work the same and have the same kind of hormone in them. Different hormonal IUDs last for different lengths of time: the Mirena and Liletta IUDs work for up to 8 years. Kyleena works for up to 5 years. Skyla works for up to 3 years.
You don’t have to keep your IUD for that many years though — you can get your IUD taken out whenever you want. If your IUD is going to expire but you want to keep using an IUD, your nurse or doctor can replace it.
What are the benefits of a hormonal IUD?
In addition to preventing pregnancy, many people use hormonal IUDs to help with period problems. Hormonal IUDs can cut down on cramps and make your period way lighter. Some people stop getting their periods at all while they have the IUD. Hormonal IUDs can also help treat the symptoms of things like endometriosis and PCOS.
There are lots of other benefits to IUDs. They’re super convenient — once your IUD is in place, you don’t have to think about birth control for several years. IUDs are also one of the most effective methods of birth control you can get. They’re more than 99% effective at preventing pregnancy. And if you decide you want to get pregnant, you can get your IUD removed whenever you want and your fertility will go back to what’s normal for you right away.
What are the disadvantages of a hormonal IUD?
Some people have side effects like spotting, irregular periods, or cramping after getting a hormonal IUD. But this usually goes away within 3–6 months, once your body gets used to your IUD.
IUDs are one of the most effective and convenient ways to prevent pregnancy, but they don't protect you from sexually transmitted infections. So use condoms with your IUD every time you have sex to lower the chance of getting or spreading STDs.
What hormones are in the different hormonal IUDs?
All hormonal IUDs use the same hormone — progestin — to prevent pregnancy and help treat painful and heavy periods. Progestin is a safe, synthetic form of a hormone called progesterone that your body makes naturally.
Mirena hormones are the same as in all other hormonal IUDs — Mirena uses progestin to prevent pregnancy and make your periods lighter and less painful. Liletta, Kyleena, and Skyla also have progestin in them.
Some hormonal IUDs have a little bit more progestin than others. But the amount of hormones in an IUD only affects how long it lasts — it doesn’t change how well your IUD prevents pregnancy. All hormonal IUDs are more than 99% effective at preventing pregnancy.
Can IUDs be used as emergency contraception?
Yes! The Paragard, Mirena, and Liletta IUDs work super well as emergency contraception. If you get one of these IUDs put in within 120 hours (5 days) after unprotected sex, it’s more than 99% effective. It’s actually the most effective way to prevent pregnancy after sex.
Another great thing about using an IUD as emergency contraception: you can keep it and have really effective birth control that you can use for up to 8 to 12 years (depending on which kind you get). The other kind of emergency contraception is the morning-after pill. You can take it up to 5 days after unprotected sex to reduce the risk of pregnancy.
What are non-hormonal IUDs?
IUD stands for Intrauterine Device — a birth control method that sits inside your uterus. A non-hormonal IUD is a small piece of flexible plastic shaped like a T that has copper wrapped around it. That’s why it’s also called the copper IUD.
Non-hormonal IUDs use copper to prevent pregnancy. Sperm doesn’t like copper — it changes the way sperm cells move so they can’t swim to an egg. If sperm can’t make it to an egg, pregnancy can’t happen.
One of the awesome things about IUDs is that they last for years, but they’re not permanent. If you decide that you want to get pregnant, or if you just don’t want to have your IUD anymore, your nurse or doctor can take it out. After you get your IUD removed, your fertility goes back to what's normal for you.
What are the kinds of non-hormonal IUDs?
There’s only one brand of copper IUD in the U.S. It’s called the Paragard IUD. It lasts for up to 12 years.
You don’t have to keep your IUD for 12 years though — you can get your IUD taken out whenever you want. If your IUD is going to expire but you want to keep using an IUD, your nurse or doctor can replace it.
What are the benefits of non-hormonal IUDs?
The copper IUD is really good at preventing pregnancy, and it’s totally hormone free. So it’s a good option for people who prefer non-hormonal birth control, or can’t use methods with hormones because of medical reasons.
The copper IUD can be used as emergency contraception — a way to prevent pregnancy AFTER unprotected sex. IUDs are the most effective form of emergency contraception. If you get one inserted within 120 hours (5 days) after having unprotected sex, it’s more than 99% effective against pregnancy. And you can leave your copper IUD in to keep preventing pregnancy for as long as you want, up to 12 years.
There are lots of other benefits to IUDs too. They’re super convenient — once your copper IUD is in place, you don’t have to think about birth control for up to 12 years. IUDs are also one of the most effective methods of birth control you can get. They’re more than 99% effective at preventing pregnancy. But if you decide you want to get pregnant, you can get your IUD removed whenever you want and your fertility will go back to what's normal for you right away.
What are the disadvantages of non-hormonal IUDs?
Non-hormonal (copper) IUDs can make your periods heavier and cause cramping, especially in the first 3-6 months. And you may have some IUD cramps when you first get your IUD. For many people, these side effects get better once your body gets used to the IUD. So if you can stick it out for a few months, there’s a good chance the side effects will ease up.
It’s normal to have some cramping during your period with a copper IUD. But if your cramps are really bad and over-the-counter medicine doesn’t help, talk with your nurse or doctor. It’s also a good idea to call your nurse or doctor if you’re still having bad IUD cramps after a year, or you have pain or IUD cramps when you’re not on your period — this can be a sign your IUD has moved, and they may want to check to make sure it’s still in place.
IUDs are one of the most effective and convenient ways to prevent pregnancy, but they don't protect you from sexually transmitted infections. So use condoms with your IUD every time you have sex to lower the chance of getting or spreading STDs.
Source: Planned Parenthood
Last updated : 1/9/2023