What is the treatment for anaphylaxis?
The first line treatment for anaphylaxis is epinephrine. It’s the ONLY medication proven to stop a life-threatening allergic reaction. Epinephrine needs to be given as soon as anaphylaxis symptoms occur.
Any delay in administering epinephrine greatly increases the chance of hospitalization. Delaying or failing to use epinephrine has been associated with fatalities.

What is epinephrine?
Epinephrine is a form of adrenaline, a hormone that naturally occurs in the body. It is also used as a life-saving medication to treat anaphylaxis. Epinephrine is given using an auto-injector or injection into the muscle in the outer thigh.
How does epinephrine work?
When epinephrine is given by injection, it increases your heart rate and blood pressure as well as relaxes the muscles in the airways. It reverses swelling and suppresses the body’s immune system’s response to allergens. Epinephrine reverses the symptoms of anaphylactic shock and temporarily halts the allergic reaction.
Epinephrine is the ONLY drug that will reverse anaphylaxis and should be given as soon as symptoms appear.
Any delay in giving epinephrine greatly increases the chance of hospitalization. Deaths due to anaphylaxis are often associated with either delaying the use of epinephrine or not using it at all.
How do you use an epinephrine injector?
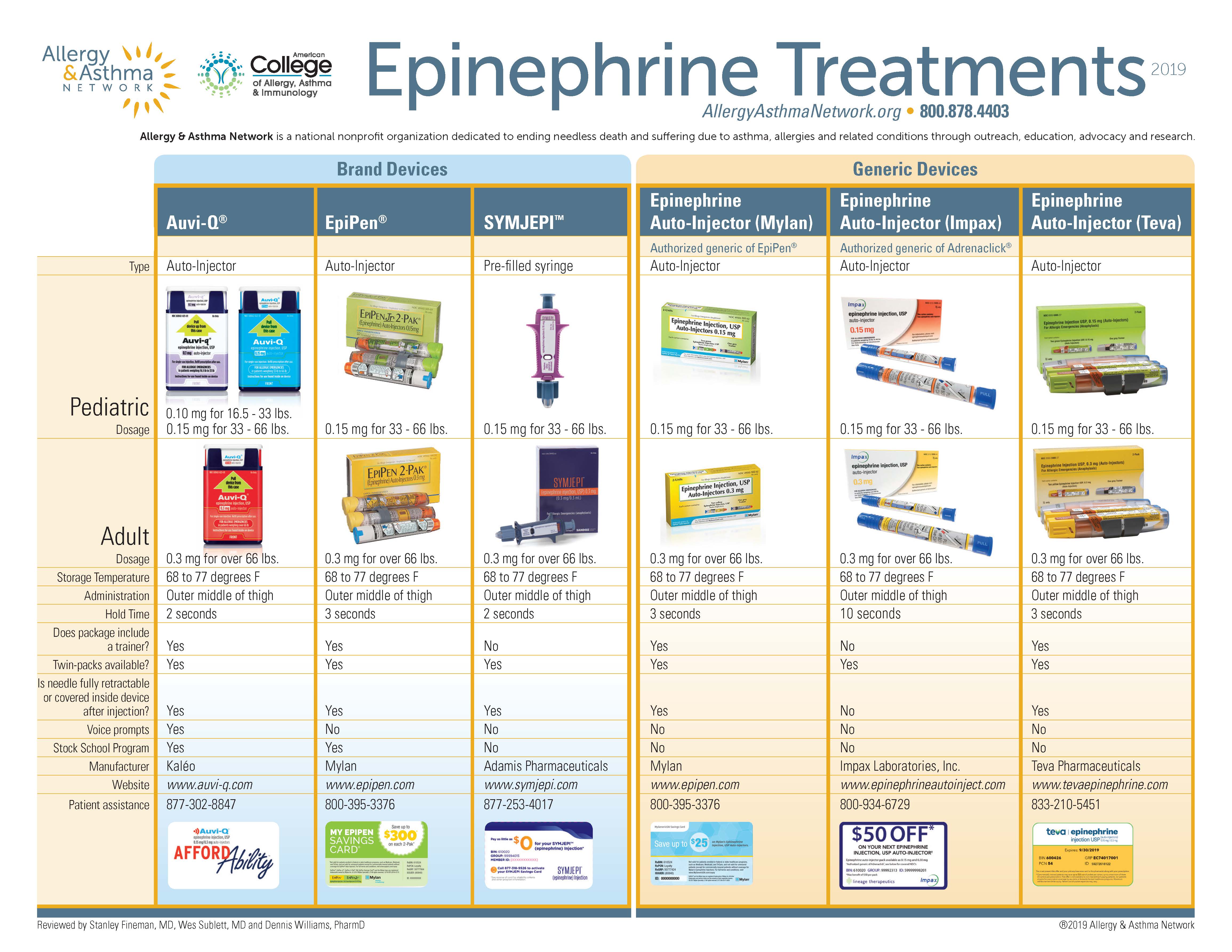
Epinephrine injectors contain a premeasured dose of epinephrine. Two different strengths are available for treating different body weights.
There are several different brands of epinephrine injectors available. Each has its own operating instructions. Be sure to visit the website of the device you are using so you can view the training video and learn how to operate the specific device you have.
Some epinephrine treatments are available as an auto-injector while some are a pre-filled syringe. Be sure you know what your prescribed device is.
General step-by-step instructions for epinephrine auto-injectors
Epinephrine auto-injectors are easy to use and come with clear instructions. The device’s needle sits protected inside the device until you inject it. Ask your doctor for training on how to correctly use an epinephrine auto-injector; manufacturers’ websites may also provide detailed steps and how-to videos.
- Pull off the safety cap or needle covering.
- Inject the epinephrine into the outer thigh; avoid the buttocks area. The needle is designed to go through clothing if necessary. Hold the leg and keep it steady while you inject the epinephrine.
- Once injected, follow the device’s instructions for how long to keep it in place — usually several seconds — until all the epinephrine is delivered.
- Remove the device and massage the injection site for 10 seconds.
- Call 911 immediately. Tell the dispatcher you just used epinephrine to treat a suspected anaphylactic reaction. Make arrangements for transport to an emergency department for additional treatment. Side effects may include uncontrollable shaking or twitchiness and feelings of panic or anxiety. These should subside within a few minutes or an hour.
Maintaining Your Epinephrine Injector
Store your epinephrine injectors as close to room temperature as possible. Leaving them in extremely hot or cold temperatures can make the epinephrine ineffective or cause the injector to malfunction. Do not store them in your car or in a refrigerator.
When outside, you need to keep your epinephrine injector close at hand, so pack it in a purse or backpack.
Keep your epinephrine injectors out of direct sunlight; this can cause the epinephrine to oxidize (combine with oxygen, changing the makeup of the drug) and become ineffective. Oxidized epinephrine will appear dark or have solid particles in it. Epinephrine can also oxidize on its own over time, so check your device regularly to be sure the liquid inside is clear.
Epinephrine injectors have an expiration date and they should be replaced as soon as they expire. (However, if all you have is an outdated auto-injector in an emergency, use it as it may provide some benefit.) Check the date on your devices regularly, including backups that may be in a school nurse’s office or at a family member’s house.
© 2021 Allergy and Asthma Network
Last updated : 12/11/2020