How do I know if my asthma is controlled?
Are you experiencing asthma symptoms on a regular basis even when following your treatment plan? Your asthma may not be in control. Use the following tools to find out more about your asthma control, then take the results to your doctor. You can use these results to discuss asthma control and your Asthma Action Plan with your doctor.
How do I prevent asthma symptoms from coming back?
Once the obvious symptoms of an asthma flare end, think about what happened in the moments, hours or days leading up to the episode. Look for clues as to what may have started the symptoms.
When you find out what triggers your symptoms, do your best to avoid those triggers. This may require a change in lifestyle, such as avoiding all exposure to cigarettes, cigars and pipe smoke; keeping pets out of the bedroom or removing them from the home; and placing dust-mite-proof encasings on your pillows and mattress. It may mean changing your furnace filters more often or removing moldy carpeting and fixing the water leak that caused it.
However, you may not be able to avoid every circumstance likely to result in asthma symptoms, such as going outside when pollen counts are high. That’s why asthma medications are a necessary part of your Asthma Action Plan.
In addition, immunotherapy (allergy shots or tablets) can teach your immune system to respond less strongly to allergens such as animal dander, dust mites, molds and pollens. If you have allergic asthma, controlling allergies will help control your asthma.
When you find out what triggers your symptoms, do your best to avoid those triggers. This may require a change in lifestyle.
When should I see an asthma specialist?
Asthma is an ever-changing condition that requires constant attention. If you continue to experience asthma symptoms that disrupt everyday activities, even after strictly following your treatment plan, then a visit to an asthma specialist is in order.
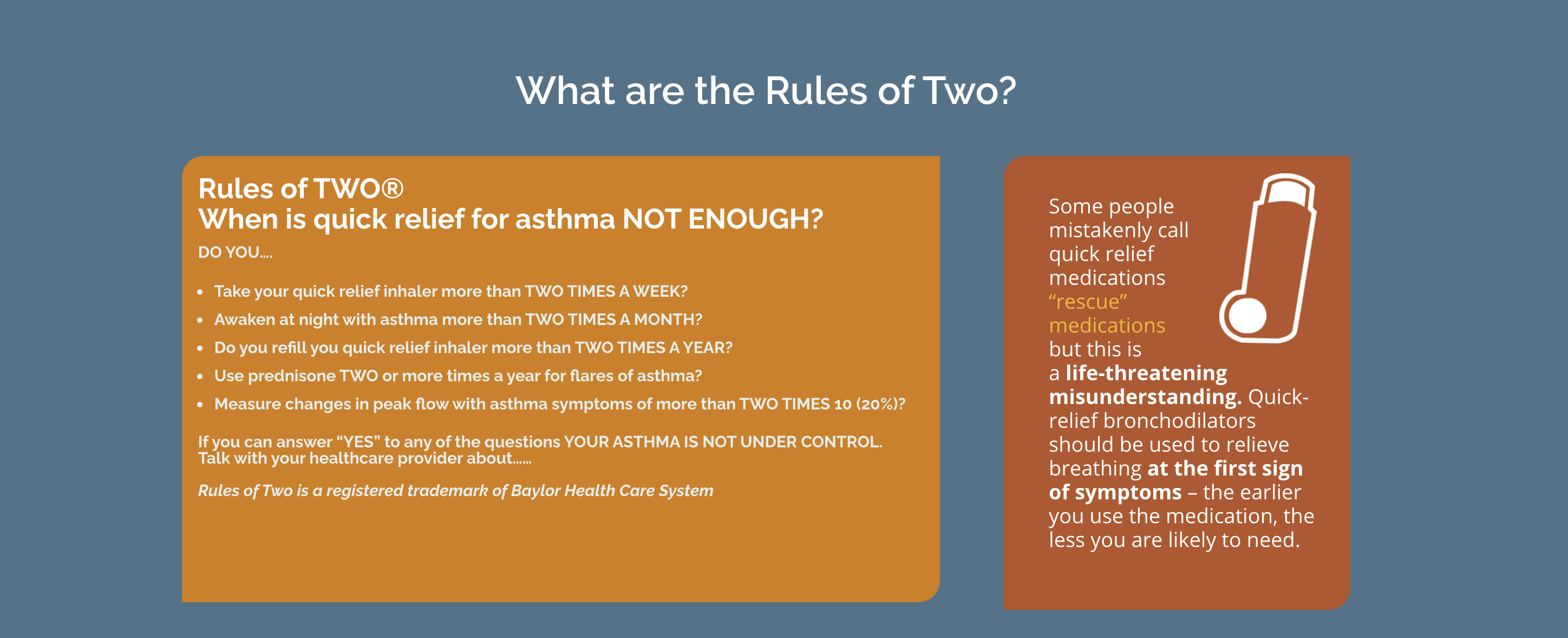
How to know if your treatment plan is not working:
- You have asthma symptoms and require use of a quick-relief inhaler two or more times a week (except to prevent symptoms before exercise).
- Your asthma wakes you up two or more times a month.
- You are refilling your quick-relief inhaler two or more times a year.
- Use prednisone TWO or more times a year for flares of asthma?
- Measure changes in peak flow with asthma symptoms of more than TWO TIMES 10 (20%)?
National asthma guidelines recommend seeing a specialist if any of the following occur:
- You have had a severe or life-threatening asthma flare.
- You are not responding to treatment after 3-6 months.
- You have persistent asthma symptoms and limited physical activity.
- You need continuous high-dose inhaled corticosteroids or more than two courses of oral corticosteroids in one year.
- You need additional testing like allergy tests, spirometry breathing tests, rhinoscopy (looks inside nasal passages and sinuses) or bronchoscopy (looks into the lungs).
- You have conditions that complicate your asthma, such as allergic rhinitis, sinusitis or GERD.
What is the September asthma peak?
September is often a challenging month for people with asthma, especially children. Studies show asthma flares and hospitalizations tend to spike in the first few weeks that children are back at school
- Why does this happen? Some factors include:
- fall ragweed pollen and mold (both are common asthma triggers)
- greater exposure to respiratory illnesses, including the common cold
- indoor allergens at school, such as mold, chalk dust and dander from school pets
- not following a treatment plan or taking prescribed medications during the summer (when symptoms are often less noticeable)
Preparation is the key to keeping your child healthy. Schedule wellness doctor appointments before school begins, make sure your child continues to take asthma medications as prescribed and review your child’s Asthma Action Plan and inhaler technique. Many schools require Asthma Action Plans be kept on file.
Are there other conditions that may look like asthma or complicate asthma?
There are other types of respiratory conditions that are different than asthma. The symptoms, diagnosis and treatment can vary depending upon the condition. Here are some of them.
- AERD
- alpha-1 antitrypsin deficiency
- bronchiectasis
- COPD
- COVID-19
- influenza, infections & viruses
- RSV
- sleep apnea
- vocal cord dysfunction
Patient education resources from Allergy & Asthma Network

© 2021 Allergy and Asthma Network
Last updated : 6/26/2024