A wide range of substances called "allergens" can trigger allergies. Allergy tests can be performed to determine which substances
Common allergy triggers include the following:
Pollen Allergy
Pollen is produced by trees, grasses, and weeds. Different plants produce pollen at different times of years, including the spring, summer and fall. Pollen allergy symptoms worsen as the concentrations of pollen increases in the air.
Allergy symptoms include sneezing, runny nose, congestions and itching, watery eyes.
Symptoms can be reduced by staying indoors on windy days or when pollen counts are high, closing windows, using air conditioning, and refraining from hanging clothes out to dry during the pollen season.
Treatment options include antihistamines, decongestants, corticosteroid nasal sprays, and immunotherapy (allergy shots).
Dust Mite Allergy

Dust mites are microscopic animals that are one of the most common causes of indoor allergies. The droppings and decaying bodies of dust mites trigger allergic reactions in susceptible people. If dust mite droppings are inhaled or come in contact with the skin, a susceptible person may experience allergic rhinitis, asthma or eczema.
Dust mites thrive in warm, humid environments where they feed on the dried scales of human skin. This means that they are found most commonly found in bedding, stuffed furniture, carpets, old clothing, and stuffed toys.
Symptoms of a dust mite allergy are similar to pollen allergy but usually occur all year rather than during specific seasons.
Dust mite allergy symptoms can be minimized by putting dust mite covers over mattresses, pillows, and box springs, using hypoallergenic pillows, and washing sheets weekly in hot water.
It can also be helpful to keep the indoor humidity below 45% and clearing the bedroom of dust collecting-items, such as stuffed animals, curtains, and carpet.
Mold Allergy
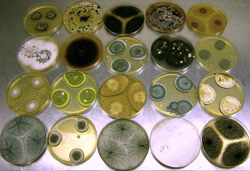
Molds grow indoors and outdoors, in all kinds of weather, and all year long. Mold allergy symptoms may worsen from July to late summer when the spores are spread by the wind.
However, there is no "mold season" as occurs with pollen allergies.
Mold counts can change quickly with the weather. Certain spore types reach peak levels in dry, breezy weather. Some need high humidity, fog or dew to release spores. This group is abundant at night and during rainy periods.
The symptoms of mold allergy are similar to those of pollen and dust mite allergies and include sneezing, congestion, itchy and watery eyes, and runny nose.
The treatment options for mold allergies are similar to those available for dust mite and pollen allergies.
Mold allergy symptoms can be controlled by avoiding activities that trigger symptoms. This might include avoiding raking leaves, keeping windows and doors closed, and making sure moist places in the home, such as the basement and bathrooms, are well ventilated. Repair areas of water damage and keep the number of indoor plants to a minimum.
Animal Allergy (Pet Dander)
Dogs, cats and birds can trigger allergies and are a common source of allergy symptoms in children. Pet allergies are triggered by the the animal's "dander", a general term that describes the different proteins shed from the animal's skin, including skin cells, fur, feathers or saliva. The bird feathers used in down pillows and comforters can also be a source of dander.
Allergies to animals can take 2 or more years to develop and symptoms may not improve until months after ending contact with the animal.
Pet allergy symptoms can be reduced by keeping pets out of the bedroom, keeping pets off upholstered furniture and washing pets weekly. In some cases, removing the pet from the home may be necessary.
Food Allergy

Foods are a common trigger of allergy symptoms. Foods that commonly trigger allergies include nuts (peanuts, cashews, walnuts and others), milk, eggs, fish, shellfish, and wheat.
A food allergy usually occurs within minutes of eating the food. Symptoms of food allergy may include asthma, hives, vomiting, and swelling in the area around the mouth. The best treatment is to avoid the offending food.
If exposed to a food to which one is allergic, treatment with antihistamines or corticosteroids is recommended.
Some people with food allergies are at risk of developing anaphylaxis and may need treatment with self-injectable epinephrine if anaphylaxis symptoms develop.
Insect Sting Allergy
Insects that commonly cause allergic reactions include bees, yellow jackets, hornets, wasps, and fire ants. Everyone will react to stings by these insects, but those with insect sting allergies will experience profound swelling and itching. They may also develop hives and are at risk of developing anaphylaxis.
The likelihood of being stung can be reduced by wearing shoes, not wearing brightly colored clothes, avoiding scented cosmetics and by keeping insecticide available.
If a person with insect sting allergy gets stung, the immediate use of an oral antihistamine, such as Benadryl, may help to minimize symptoms. It is important to monitor for signs of anaphylaxis and call 911 if they develop. Self-injectable epinephrine (EpiPen®) may need to be administered if available.
Insect stings are usually accidental and cannot always be prevented. Allergy shots may be recommended for some to help prevent the risk of developing anaphylaxis.
Medication Allergy
Some medications, such as sulfa, penicillin and aspirin, can trigger allergic reactions. Symptoms of a drug allergy can range from mild to life-threatening and may include a skin rash called a "fixed drug eruption", hives, swelling in the mouth and throat and general nasal congestion.
The treatment of drug allergies includes avoiding medication and administering antihistamines or corticosteroids after exposure. Bronchodilators may be prescribed for asthma symptoms. Those at risk of developing anaphylaxis may need access to self-injected epinephrine.
Latex Allergy
Latex gloves are the most common offending product for people with a latex allergy.
Latex, found in latex gloves, condoms or certain medical devices, can trigger allergy symptoms, including a rash, eye irritation, runny nose, and asthma symptoms. Symptoms can range from from skin redness and itching at the site of exposure, to anaphylaxis.
Treatment of latex allergy includes avoiding exposure to latex. If you have a latex allergy, you may be advised to wear a MedicAlert bracelet and carry self-injectable epinephrine with you at all times. If exposed to latex, antihistamines or epinephrine may be administered.
Source: Vivacare
Last updated : 4/19/2023