How common is latex allergy?
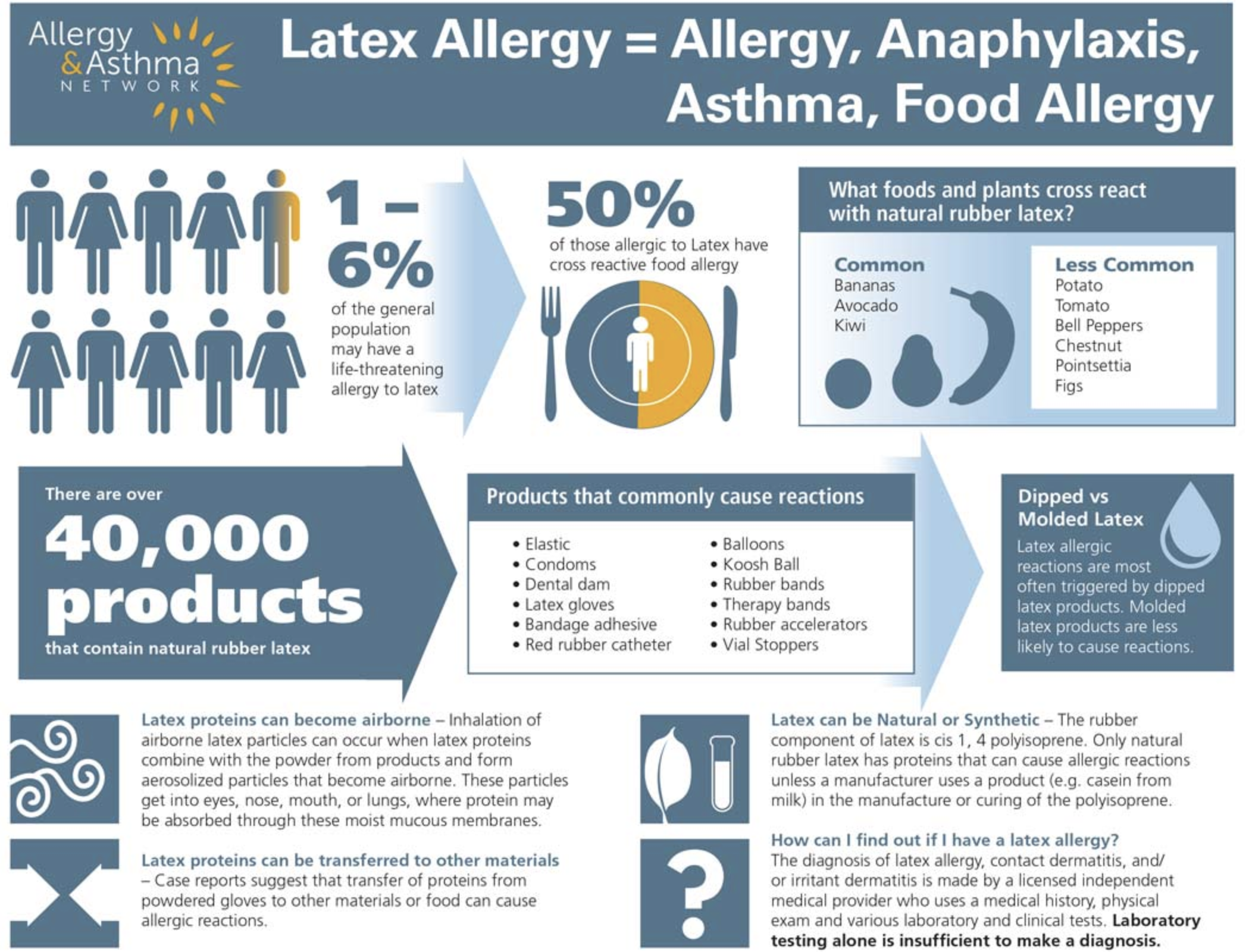
While latex allergy is rare, affecting 1 to 6 percent of the general population, it is much more common in employees who work in the medical or dental health field.
In fact, 10-17 percent of healthcare workers and 33.8 percent of dental care workers have been diagnosed with latex allergy. In addition, 17 percent of restaurant workers have been diagnosed with latex allergy.
People who undergo multiple surgeries – such as spina bifida patients – are also at increased risk for latex allergy.
What are the different types of latex allergy?
There are three types of reactions to natural rubber products.
- IgE-mediated allergic reaction (Type I)
- allergic contact dermatitis (Type IV)
- Irritant contact dermatitis.
Cell-mediated contact dermatitis (Type IV)
Cell-mediated contact dermatitis is an allergic contact dermatitis. A Type IV cell-mediated reaction is not life-threatening but it is still a major concern. A cell-mediated reaction is usually limited to the skin where contact occurs with rubber products. The rubber products contain numerous chemicals used in its production that can cause a reaction in some people.
This type of contact dermatitis is a delayed type immune reaction. Symptoms may take 24-48 hours to develop from the time of exposure to reaction.
Symptoms of Type IV allergic contact dermatitis reactions are confined to the skin:
- a red rash
- papules – an elevation in the skin that is solid and can be colored – many papules together appear as a rash
- vesiculation – a blister-type rash
- oozing
If someone is repeatedly exposed with a Type IV reaction, the rash may develop into a chronic problem and may even extend beyond the site of contact.
People can have both a delayed contact allergy to chemicals in latex along with an IgE-mediated allergic latex allergy.
Irritant contact dermatitis
Individuals who use rubber products frequently (for example, healthcare workers who wear gloves) may develop irritant dermatitis.
This dermatitis is different from allergic contact dermatitis. It is not mediated by an immune system sensitization and reaction. Rather, it is caused by frequent skin washing, sweating and/or irritation from powder lubricants.
This rash may be itchy, but most commonly is dry, red, and accompanied by skin cracking. There are rarely papules, vesiculation or oozing of the skin. It never extends beyond the point of contact with the offending irritant.
There are two major categories of natural rubber latex:
- Dipped – These products are stretchy rubber and usually contain the highest content of latex proteins (gloves, balloons, condoms).
- Molded – These products are dry-molded to be hardened rubber products (vial stoppers, syringes, gaskets).
Synthetic rubber latex products do NOT contain natural rubber latex proteins but may contain rubber accelerators that are used in manufacturing. If you are sensitive to accelerators, you may have a synthetic rubber latex reaction.
What are the symptoms of latex allergy?
Latex allergy (Type I) symptoms range from skin irritation to respiratory symptoms to life-threatening anaphylaxis – and there’s no way to predict which will occur if exposed.
Symptoms of latex allergy may be mild at first, progressing to more serious types of symptoms.
Symptoms of latex allergy include:
- skin redness
- urticaria (hives)
- itching
- nasal drainage
- sneezing
- itchy eyes
- throat irritation
- asthma
A latex allergy reaction can also result in anaphylaxis, a life-threatening allergic reaction.
Symptoms can start within seconds of exposure to latex or may not appear until hours later. The allergic reaction can be different each time a person experiences anaphylaxis and can vary in severity each time. Once the reaction starts, it usually progresses quickly. This makes identifying anaphylaxis and responding to care tricky at times.
A board-certified healthcare professional, often an allergist, makes the diagnosis of latex allergy, as well as contact dermatitis and/or irritant dermatitis. The healthcare professional uses a combination of medical history, physical exam and various laboratory and clinical tests. Laboratory testing alone is not enough to make a diagnosis.
Patients are encouraged to provide a full list of items and foods that may have caused a latex-allergic reaction to help determine whether latex allergy is present.
How is latex allergy diagnosed?
Allergy to latex may be challenging to diagnose and treat.
If you suspect you have a latex allergy, consult an allergist. Be prepared with as much medical history as possible, including where you were and what latex products you were exposed to when you experienced a reaction.
The diagnosis of latex allergy, contact dermatitis and/or irritant dermatitis is made by an allergist after completing these three parts of an evaluation:
- medical history
- physical exam
- various laboratory and clinical tests
Laboratory testing alone is not enough to make a diagnosis. There is a blood test available, but the results are not 100 percent accurate.
Latex-specific IgE antibodies can be identified through skin testing or by blood tests. (Patients should be aware that skin testing for latex allergy has a small risk of adverse reactions.) There is no FDA-approved skin test reagent for latex allergy in the United States.
Contact dermatitis is confirmed by the use of patch testing.
Irritant dermatitis is diagnosed by the patient’s medical history and a physical examination.
How do you prevent a latex allergy reaction?
Treatment for a latex allergy involves avoidance of the source of latex that causes the reaction.
In the case of IgE-mediated allergy, personal contact with rubber products should be stopped and a change of environment may be necessary if there is airborne exposure causing asthma or occupational asthma.
This is most prominent in settings that use cornstarch powdered latex gloves. Cornstarch powder serves as a carrier for allergenic proteins from latex. It may become airborne when the product is used. These protein particles can easily become airborne and people with latex allergy may experience a reaction if the powder is inhaled or comes in contact with the mucus membranes of the eyes, nose or skin.
Some latex products are more allergenic than others. Latex products most likely to cause a reaction are those made by a dipping method (gloves, condoms, balloons). However, molded, vulcanized rubber products (tires, for example) also maintain latex allergen proteins.
How do you treat a latex allergy reaction?
Latex allergy treatment depends on the type of reaction that is present – a mild sensitivity or a life-threatening allergic reaction, or anaphylaxis.
- Anaphylaxis: Epinephrine, a medication given by injection that works quickly to raise blood pressure and reduce swelling in the body, is the first-line treatment for severe allergic reactions. It’s available in an easy-to-use epinephrine auto-injector – a prefilled syringe with a retractable needle. Epinephrine should be administered without delay when symptoms appear.
- Mild Sensitivity: If a mild sensitivity is present and there is only a local reaction – the skin is itchy and red at the site where latex was touched – your doctor may suggest using an antihistamine or using 1% hydrocortisone cream.
NOTE: Treatments mentioned here are for informational purposes only. If you have a latex allergy and require treatment, you should see a board-certified allergist to determine the best treatment for you.
Is latex allergy preventable?
Latex allergy is preventable but not curable. Awareness and education are the keys to managing the condition.
The only way for people with latex allergy to prevent symptoms is strict avoidance of latex. Allergy & Asthma Network supports policies where latex gloves are prohibited from use in healthcare and dental facilities, schools, food establishments, and by emergency responders. Many facilities have responded by switching to latex-safe gloves and medical products and supplies.
What items contain latex?
There are more than 40,000 products worldwide that contain latex and it’s often very difficult for people with latex allergy to perform everyday tasks and live a full, active life. Latex allergy generally develops after repeat exposure to medical and consumer products containing natural rubber latex.
The difficulty in managing latex allergy is that latex and latex proteins are found in so many common everyday products. For example, your daily mail may be wrapped in a rubber band; there may be a celebration that includes latex balloons; or the elastic waistband on underwear may cause a sudden and unexpected allergic emergency.
Additional products made with latex include:
- Balloons
- Rubber or latex exam gloves
- Condoms
- Elastic bands, physical therapy bands, rubber bands
- Dental dams
- Stethoscopes and blood pressure cuffs
- Spandex
- Pacifiers and baby bottle nipples
- Mouse pads
- Goggles
- Bathmats
- Garden hoses
- Certain mattresses
What foods are related to latex?
People with latex allergies may also develop allergic reactions to some fruits and vegetables. About half of people with a latex allergy may develop allergy symptoms from avocado, banana or kiwi.
This happens due to cross reactivity. Some of the proteins in natural rubber latex are similar to those found in cross-reactive fruits and vegetables.
At the same time, people with food allergies to certain fruits and vegetables may have allergic reactions to latex. This may occur in approximately 10% of food allergic individuals.
What do you do if you have a latex allergy?
- Wear Medical Identification
- Carry with you at all times:
- Medications, as prescribed by your allergist (including anaphylaxis medications: two epinephrine auto-injectors; allergy medications: antihistamines; asthma medications: inhaler/albuterol)
- Non-latex gloves
- Latex Allergy Action Plan developed with your allergist.
- Notify the following of your latex allergy and other pertinent information:
- Medical and dental providers
- Family members, friends, employer and co-workers
- EMS (if calling 911)
- Avoid:
- Natural rubber latex gloves, balloons, condoms and other natural rubber products
- Be aware of and consult with your allergist regarding:
- Proper use of medications
- “Hidden” latex on food prepared with latex gloves
- Lactiferous plants that may have cross-reactive proteins
- Foods with cross-reactive proteins to natural rubber (banana, avocado, kiwi, chestnut)
- Carry a list of medications prescribed by your allergist
Can you eat at restaurants with a latex allergy?
For individuals with latex allergy, the challenge at restaurants is threefold:
- kitchen staff may use latex gloves while preparing food
- some foods have cross react with latex proteins
- restaurants may have latex balloons on display for parties or in banquet rooms
What can you do to safely navigate restaurants with a latex allergy?
First, share your latex allergy diagnosis with the hostess or manager. Find out if the kitchen staff uses latex gloves during any aspect of food preparation. If so, emphasize the severity of your allergy and the potential consequences if you are exposed – you want to grab their attention.
Check out websites and menus of any restaurant you plan to visit. Many restaurants have already adopted a non-latex policy. This list includes Burger King, Quizno’s, Denny’s, Red Lobster, Outback Steakhouse, Red Robin, Arby’s, Subway, Bahama Breeze, Domino’s Pizza and Cracker Barrel Old Country Store. Disney World and Disneyland also have adopted a non-latex policy.
Higher risk situations are establishments with buffets (risk of cross contamination), pre-made foods (unable for the chef to eliminate an ingredient) and eateries that frequently use banana, kiwi or avocado. Look for restaurants that have food allergy training for employees.
Notify the hostess and server of your latex allergy and review the menu for dishes that are unsafe. Bring a “chef card” with details of your allergy that the server can hand to the chef. By submitting this card, you don’t have to rely solely on verbal communication passing from server to chef.
Latex-allergic individuals should carry two epinephrine auto-injectors, wear medical identification and pack a copy of a letter from an allergist detailing the diagnosis and what to do in case of an emergency.
How to navigate restaurants with a latex allergy
The frenzied pace of working in a restaurant requires every member of the staff – from hostess, executive chef, manager, line cook and server – to be familiar with food and latex allergies, and to work together to ensure food service is safe.
Call the restaurant, ask for the manager or host, and discuss your latex allergy. Ask if the restaurant has latex balloons on display and if kitchen staff uses latex gloves during any part of food preparation.
Emphasize the severity of your latex allergy and the potential consequences if you are exposed to latex.
What are important things to know about latex allergy and schools?
Providing a safe environment for students at school goes beyond food and environmental allergies – latex allergy must also be considered. In the school setting, we often see latex allergies in children who have experienced multiple medical procedures, especially children with spina bifida.
Latex appears in items commonly used in school, including many brands of erasers, balloons, rubber bands, gloves, balls and mats used in physical education. The school needs to identify latex-free school products and latex-free sports equipment when a student has an allergy.
All members of the school community should collaborate to manage latex allergy by:
- Educating the school community
- Identifying potential exposure to latex
- Preparing to respond in an emergency
- Creating a plan for the future
What are important things to know about latex allergy and vaccines?
Some vaccine packaging contains latex, posing a threat to people who have a latex allergy. There is concern that latex proteins may be mixed with the medication through packaging and storage of the vaccine vial, and also through puncturing the vial stopper to “draw up” the vaccine. The same concern exists with vaccines that are stored in syringes with latex in the plungers.
While the extent of the risk is unknown, it is difficult to be sure how much latex may be present in a vaccine package. Since current recommendations are based on limited data, patients should talk with their allergists to determine the best approach to obtaining a needed vaccine.
Current strategies can include:
- “Popping the top” prevents the puncturing of a latex stopper for safer administration. However, there is still a possibility that latex allergic proteins contaminated the medicine during the period of storage.
- The “one stick rule” is based on the assumption that a single stick through the vial seal minimizes latex allergen distribution into the medication, while maintaining a closed system that limits potential for contamination.
- Post-vaccination observation by a qualified individual for a period of at least 15 minutes, and up to two hours.
Can Poinsettia Plants cause latex allergy reaction?
The poinsettia plant, used for holiday decorating, is botanically related to natural rubber latex. When the leaves or stems are broken, it releases a milky white substance that can cause reaction in latex allergic individuals.
© 2021 Allergy and Asthma Network
Last updated : 12/11/2020