You may need to speak to your doctor if routine skin care measures and over-the-counter remedies are not sufficient for keeping your eczema symptoms under control
Your doctor will recommend an eczema treatment plan based on several variables, including:
- the type or cause of your eczema
- the location of the rash (face vs. knee)
- the severity of eczema and its impact on your life
- the duration of symptoms (acute vs. chronic). Long-lasting symptoms usually require more potent eczema medications.
- Results from previous treatments
- Your personal preferences
The goals of eczema treatment are to heal the skin, prevent new flare-ups, and reduce itching and urge to scratch, which can lead to even greater problems.
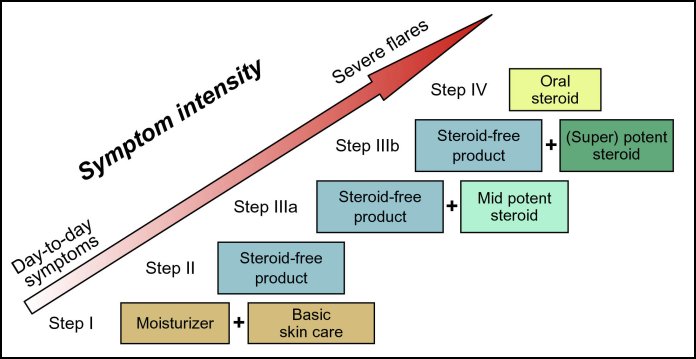
There are a variety of eczema medications available that can be categorized as follows:
- Topical corticosteroids
- Calcineurin inhibitors (Elidel®, Protopic®)
- Antihistamines
- Antibiotics
- Oral corticosteroids (prednisone)
- Immunosuppressants (cyclosporine)
These medications may be added or removed from the recommended treatment plan in a step-wise fashion depending on symptom intensity.
Eczema treatment may need to be sustained for many months to bring it under control, and eczema treatments often need to be repeated.
Eczema and Skin Care
It is critical that basic skin care measures be maintained in order to keep atopic dermatitis under control. Basic steps include avoiding substances that trigger eczema, selecting and using appropriate skin care products and frequent moisturizing.
One of the most important steps for treating and managing atopic dermatitis is to use a moisturizer. Moisturizers provide a layer of protection from irritants, trap moisture in the skin, help restore the skin barrier, and improve the skin’s appearance.
Regular use of a moisturizer for eczema may reduce the need for other medicines.
Moisturizers are best applied at least twice a day within 3 minutes after a bath, shower, or swim.
When choosing an eczema moisturizer, look for a hypoallergenic and ointment-based product. Thicker moisturizers will protect the skin longer than lighter lotions. Avoid moisturizers containing alcohol, fragrances, or other chemicals that can irritate the skin. Even seemingly harmless substances like glycerin can dry the skin of people with atopic dermatitis.
Brand names of frequently recommended moisturizers include:
- CeraVe®
- Cetaphil®
- Eucerin®
- Aquaphor®
- Vaseline® Petroleum Jelly—-though thick, it is quickly absorbed by very dry skin
Before applying the moisturizer for eczema, use tepid water and a gentle cleanser to remove dead skin cells. Do not scrub or rub excessively. Apply the moisturizer immediately afterward while the skin is still damp.
Remember to use plenty of moisturizer to keep atopic dermatitis at bay, especially in children. Keeping a child’s skin sufficiently moisturized could require as much as 1-2 bottles of moisturizer per week. Adults will need even more.
Bleach Baths
Bleach baths may be recommended for some individuals, particularly children, to help keep eczema under control and to reduce the chance of developing skin infections, such as impetigo.
Eczema Medications
Topical corticosteroids
Topical corticosteroids are commonly used to calm the irritation from an eczema or atopic dermatitis flare. These anti-inflammatory medications are available in various strengths, with “super potent” being the strongest. The more potent, the greater the risk of side effects.
Mild or acute cases of atopic dermatitis usually respond well to mild corticsteroids. Severe or chronic atopic dermatitis, with skin thickening, or on the palms or soles, may require more potent corticosteroids.
If topical corticosteroids are used for too long or inappropriately, they can cause side effects such as thinning of the skin, or become absorbed into the blood.
Use only mild corticosteroids on delicate areas like the face, groin, underarms, and genitals. Potent formulations should only be used for a few weeks at a time and never on wounds or skin that is thinned from overuse. Potent corticosteroids should be used with special care in children.
In general, moderate-to-potent corticosteroids are recommended for use on thick lesions for a limited time.
Calcineurin Inhibitors (Elidel®, Protopic®)
Calcineurin inhibitors (TCIs), also called "topical immunomodulators", are a type of medication applied to the skin that can help control the symptoms of atopic dermatitis and reduce the need for topical corticosteroids. They are a useful alternative for sensitive locations, such as the face and skin folds. They are generally effective and well tolerated.
There are currently two FDA-approved topical immunomodulators for treating atopic dermatitis: Elidel® (pimecrolimus) and Protopic® (tacrolimus). Both work by reducing inflammation and other symptoms of atopic dermatitis. These medicines have fewer side effects than topical corticosteroids, but it has been theorized that they may lead to an increase risk of skin cancer.
Antihistamines (Benadryl®, Atarax®)
Oral antihistamines help reduce the itching and scratching of eczema that can further damage the skin. They are often recommended for use at night to help prevent scratching during sleep, and some people find them too sedating for use during the day.
Antibiotics
Bacteria, such as staph, can live on the surface of skin without causing any problems. However, at times, these bacteria can trigger atopic dermatitis flare-ups or prevent inflamed skin from healing.
Topical antibiotics are useful because they can be applied directly to an inflamed area. However, an oral antibiotic, such as cephalexin or erythromycin, may be recommended if larger areas are inflamed or appear infected,
Oral corticosteroids
Short courses of oral corticosteroids, such as prednisone, may help control a severe case quickly. Risks of this treatment include a rebound of symptoms and side effects such as dizziness or fatigue. The medication is usually limited to a few weeks and the dosage is often tapered off.
Immunosuppressive drugs
When atopic dermatitis fails to respond to any other therapies, immunosuppressive drugs may be recommended to calm the immune system. These include cyclosporine, methotrexate, azathioprine, and mycophenolate (Cellcept®).
Source: Vivacare
Last updated : 1/8/2019